
Most people have heard of type 1 diabetes, type 2 diabetes, and gestational diabetes, but did you know there are actually many other different types of diabetes?
The three different types of diabetes mentioned above are the most commonly diagnosed, but there are many other types as well. Keep reading to learn more about 6 different types of diabetes.
What is diabetes exactly?
Diabetes mellitus consists of several metabolic disorders that affect insulin production, the action of insulin, or both. Insulin is produced by the pancreas to allow glucose to enter your body’s cells and can then be used as energy.
When glucose levels in the blood increase, the pancreas releases insulin into the bloodstream. Insulin then attaches to the body’s cells and allows the glucose to enter and to be metabolized and used as energy.
In patients living with diabetes mellitus, insulin is either not produced or unable to attach to the cell to allow glucose to enter. In this case, glucose will build up in the bloodstream. This buildup of glucose can cause a variety of health complications if not treated.

A serious complication of diabetes
Having increased glucose in the bloodstream for an extended period of time can affect different parts of the body. One of the most serious effects of high glucose levels is called diabetic ketoacidosis (DKA). DKA is an acute and serious side effect of high glucose levels that can lead to life-threatening consequences.
When the cells are not able to use the glucose in the blood, the liver tries to produce the energy for the body. It uses body fat to do this. When fat is oxidized for energy, the byproduct is ketones. The build-up of ketones causes the blood to be more acidic leading to diabetic ketoacidosis (DKA). The symptoms of DKA are thirst, frequent urination with high ketone levels, and high blood glucose. If you have any of these symptoms, seek medical attention immediately.

Other diabetes complications
If glucose levels stay high for a long period of time, it can affect certain organs, such as your eyes, kidneys, nerves, and heart. These issues normally start within your blood vessels in these areas of the body.
Think about the last time you made coffee with sugar. You added a teaspoonful, stirred your coffee and tasted it, but it still wasn’t sweet enough. So you stuck the coffee-soaked spoon back into the sugar. The coffee caused the sugar in the sugar tin to get sticky and clumpy.
Now, apply this analogy to your blood vessels. When there is an abundance of glucose in your blood vessels it begins to clump up and stick to the walls of your blood vessels. This is where many organ issues stem from.
- Eyes: Hyperglycemia can cause retinopathy, this can cause blurry vision or even sight loss.
- Heart: The damage to the blood vessels can decrease the amount of oxygenated blood flowing through your body which puts stress on your heart. This stress can lead to a stroke or heart attack.
- Nerves: This lack of oxygenated blood flow can also cause damage to your nerves resulting in neuropathy and a lack of feeling in fingers and toes.
- Kidneys: Kidneys can get overwhelmed by the amount of glucose being filtered through them leading to more blood vessel damage in the kidney. This can lead to a kidney disease called diabetic kidney disease.
Although these situations take longer to become serious, continuous high blood glucose can cause serious damage to your body.

How many different types of diabetes are there?
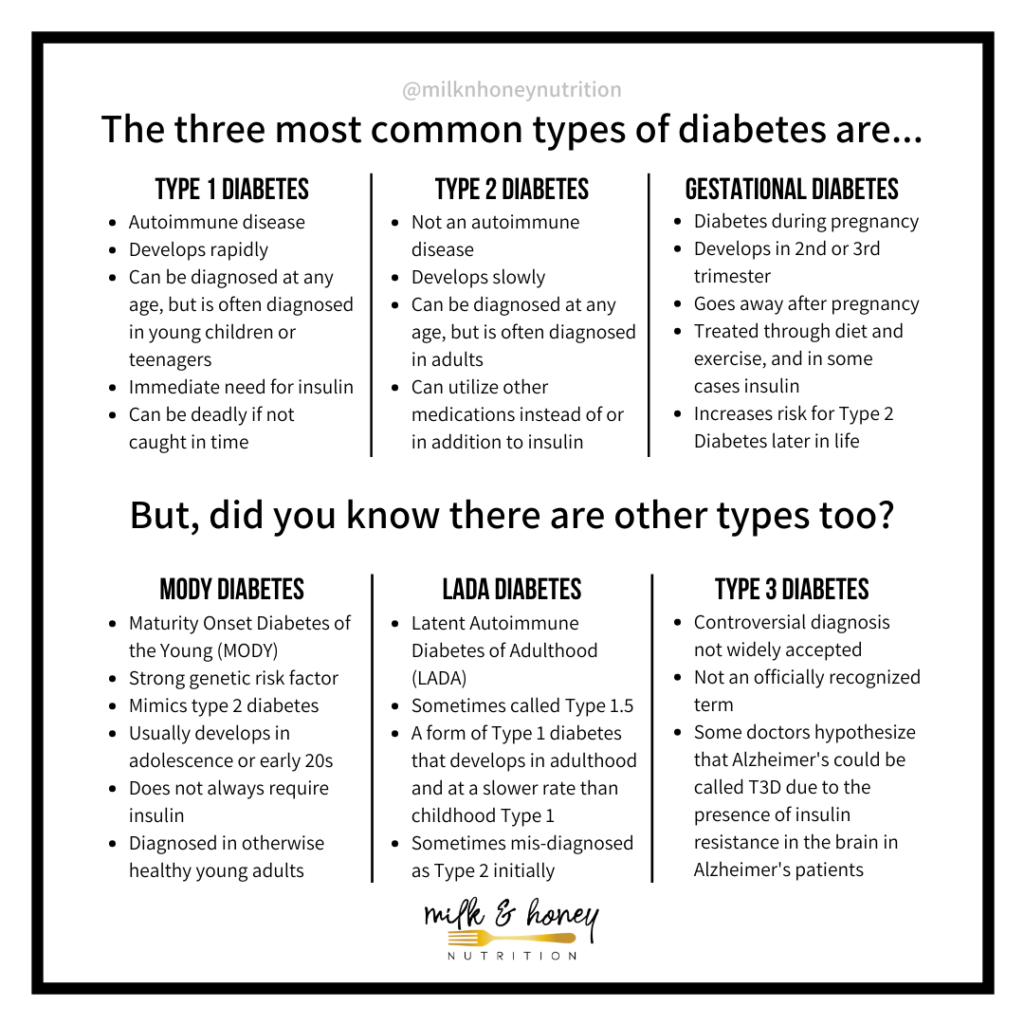
Most people are aware of type 1 diabetes, type 2 diabetes, and gestational diabetes, but there are actually many types of diabetes. There are 6 different types of diabetes we see commonly diagnosed today.
What are the 6 types of diabetes mentioned above?
Type 1 Diabetes
Type 1 diabetes is an autoimmune disease. In this type of diabetes, the body has auto-antibodies that destroy the cells of the pancreas that produce insulin. As these cells decrease, the ability to create insulin decreases. The dwindling amount of insulin causes glucose to build up in the blood.
In order to lower glucose levels, another source of insulin must be introduced to the body. This outside source of insulin can come from a vial and syringe, a pump, or a pen. If type 1 diabetes is not caught in time, the high levels of glucose can lead to ketoacidosis and can be deadly.
A common misconception of type 1 diabetes is that it is only diagnosed during childhood and early adolescence. This is not the case. Type 1 diabetes can occur at any age, but it is most often diagnosed at a younger age.
The destruction of the beta cells vary from person to person. Some people may have a gradual decrease in beta cells, while some lose the functioning beta cells extremely quickly. The period of time after diagnosis, when the pancreas is still capable of producing some insulin is called the honeymoon phase. During this phase, an outside source of insulin is necessary, but as the body continues to reduce the amount of insulin it is able to produce, insulin levels will need to be adjusted.

Type 2 Diabetes
The second type of diabetes we are going to talk about is type 2 diabetes. This type of diabetes accounts for about 90 to 95% of the people living with diabetes. Type 2 diabetes was previously referred to as adult-onset or non-insulin dependent diabetes. This type of diabetes is not insulin-dependent initially like type 1 diabetes, instead, it is notable for insulin resistance.
Cells stop responding to the insulin in the bloodstream causing a build-up of glucose in the blood. As glucose levels rise, the pancreas begins to produce more and more insulin, but the cells are still not responding. As this cycle continues, the cells that produce insulin in the pancreas can become damaged and reduce the amount of insulin produced all together. If these cells (called beta cells) become too damaged an outside source of insulin may be needed.
Type 2 diabetes has been associated with a higher percent of body fat around the abdomen, which can be associated with insulin resistance in some people, but not all.
In the early stages of diagnosis, medication or lifestyle changes can prevent the progression of the disease.
In later stages of the disease, insulin may be needed to manage glucose levels. Some other risk factors for developing type 2 diabetes are age and a lack of physical activity. There is also a genetic aspect with type 2 diabetes, along with individuals with high blood pressure and abnormal lipid levels.
There are significant racial disparities that exist both in type 2 diabetes incidence and type 2 diabetes outcomes. According to a 2020 report by the CDC “ [the] Prevalence of diagnosed diabetes was highest among American Indians/Alaska Natives (14.7%), people of Hispanic origin (12.5%), and non-Hispanic [Black Americans] (11.7%).”
Type 2 diabetes is most common in adults, but can also occur in children and adolescents. It is also worth noting that the term pre-diabetes, also mean pre-type 2 diabetes.
Gestational Diabetes
Gestational diabetes is a type of diabetes that is developed during pregnancy. A hormone that is produced by the placenta during pregnancy can reduce the body’s ability to use insulin effectively. Unlike type 1 diabetes, this is not caused by the lack of insulin, but by insulin resistance, more closely resembling type 2 diabetes.
Some of the risk factors involved in gestational diabetes are a family history of diabetes, prediabetes, age, and percentage of body fat before becoming pregnant. All pregnant women are screened at least once during pregnancy, normally within 24 to 28 weeks of gestation.
Treatment for gestational diabetes can include diet and exercise and in some cases may require insulin injections. Gestational diabetes symptoms dissipate after delivery, but having gestational diabetes increases the risk of gestational diabetes in later pregnancies and increases the risk for the development of type 2 diabetes later in life.
MODY Diabetes
MODY stands for maturity onset diabetes of the young. MODY diabetes is an inherited disease that is caused by a genetic mutation. There is a strong genetic risk factor, in fact, if a person living with MODY diabetes has a child, the baby has a 50% chance of also having MODY diabetes. Having this gene mutation affects the development of cells in the pancreas and the pancreas’s ability to produce insulin. This type of diabetes can be present in adolescents and usually is present before the age of 25.
Many MODY diabetes cases are often misdiagnosed as type 2 diabetes. Perhaps the most helpful tool in determining if the patient is living with MODY diabetes is a family history of the disease. If this information is not available there are ways to rule out type 1 and type 2 diabetes.
A way to distinguish between type 1 diabetes and MODY diabetes is the presence of antibodies. A blood test that does not have the antibodies present in type 1 diabetes can rule out this diagnosis. Ruling out type 2 diabetes can be a little more complicated. The presence of insulin resistance can help determine if the high glucose levels are due to MODY diabetes or type 2 diabetes.
There is a range of different types of MODY diabetes and treatment may be different for certain types. For instance, MODY 2 is often treated with diet and physical activity while other types of MODY diabetes will require more invasive treatments. Like all people living with diabetes, management will be individualized. Some treatment plans involve diet and exercise, some involve insulin, some involve oral medications, and some treatment involves a combination of the three.
LADA Diabetes
LADA diabetes stands for latent autoimmune diabetes of adulthood and is sometimes referred to as type 1.5 diabetes. LADA diabetes is sometimes misdiagnosed for type 2 diabetes because of the adulthood diagnosis and the possible presence of insulin resistance. It can also resemble type 1 diabetes because of the presence of autoantibodies.
If LADA diabetes is misdiagnosed it can lead to insufficient management of glucose levels and cause harm to the patent. Possible ways to distinguish LADA diabetes from other types are age, autoantibodies, and treatment.
Type 3 Diabetes
Type 3 diabetes is a somewhat controversial diagnosis and not an officially recognized term. This unofficial type of diabetes is a form of diabetes that is associated with Alzheimer’s disease. Researchers are investigating the inability of the brain to respond to insulin in Alzheimer’s patients. When the neurons of the brain are not able to respond to insulin, simple tasks such as learning and memory can be affected. Researchers are beginning to study and test a new nasal spray containing insulin on the symptoms of patients living with Alzheimer’s. This is a type of diabetes that definitely requires more research!

Some other rare types of diabetes
Other forms of diabetes include:
- Cystic Fibrosis-related diabetes
- Diabetes as a complication of Cushing’s Syndrome
- Antiretroviral associated diabetes
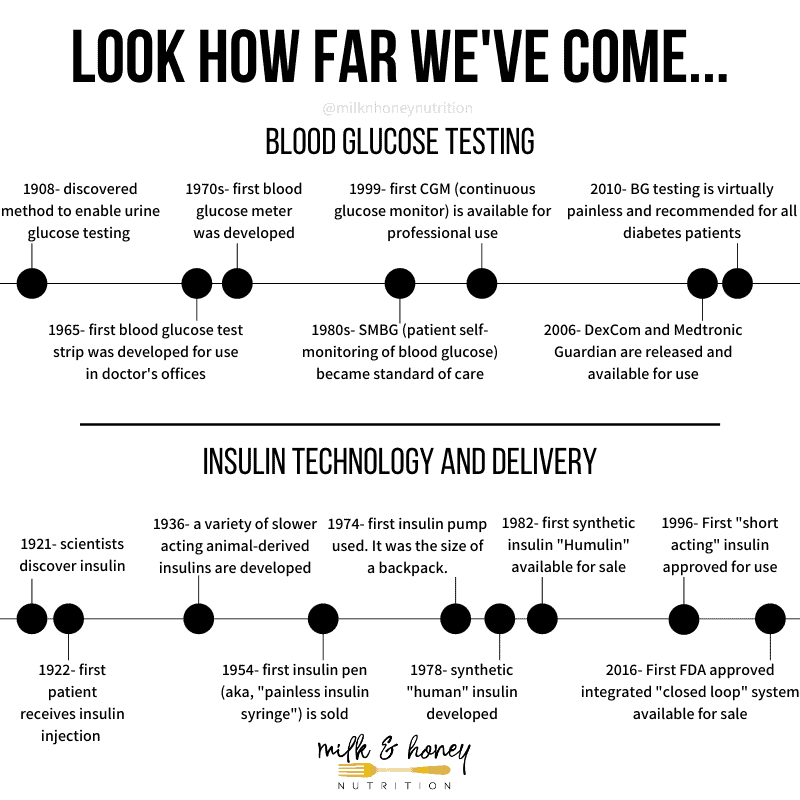
A brief history of diabetes management for different types of diabetes
All of the different types of diabetes we have discussed require blood glucose monitoring. Some require insulin immediately, and some require insulin in more advanced stages of the diabetes. The chart below gives you a quick look at the relatively recent timeline in diabetes treatment. It wasn’t until the last 100 years that people with diabetes could live long and prosperous lives!
Is diabetes a chronic disease?
All of the different types of diabetes (except GDM) discussed above are considered “chronic diseases.” A chronic disease is a health condition that lasts for one year or more and requires ongoing medical attention.
Can diabetes be cured?
There is no cure for any of the different types of diabetes we have discussed. We can, however, manage all of these types of diabetes. Some (type 2, pre-diabetes, etc.) can go into remission, but to say a person is cured of diabetes would be mis-leading.
And, regardless of what type of diabetes you or a loved one has, remember that a vibrant and joyful life is still very much possible thanks to modern day technology and insulin advancements! And if you’d like to learn just how easy and delicious cooking for diabetes can be, make sure to grab a copy of my cookbook The Easy Diabetes Cookbook!




2 Responses
This website is AMAZING ! As a person with diabetes, I struggle to find good easy to understand information about how to manage my diabetes. As a nurse, I struggle to find good easy to understand information about how to help my patients manage their diabetes .
I will be using this resource daily now !!
Thank you so much !
This site is very informative!!! Thanks